iop corneal thickness measurements|iop correction factor chart : wholesalers Background and objective Due in part to its effect on intraocular pressure (IOP) measurements, the assessment of central corneal thickness (CCT) is recognized as an essential part of the . WEBFind out all you need to know about online gambling. 888 Online Casino Review for Canadian players in2024 - 888 is a legit, certified & trusted casino. It offers 1,000+ casino games & great bonus options.
{plog:ftitle_list}
A locução adverbial «ao meio» está correta, se pretende dizer que dobra uma folha ou a corta em duas partes iguais. A referida locução está registada no Vocabulário da Língua Portuguesa (1966), de Rebelo Gonçalves, que também classifica «ao meio de» como locução prepositiva; e no Grande Dicionário da Língua Portuguesa de José Pedro .
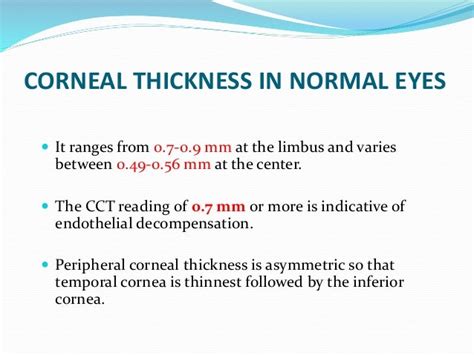
iop Intraocular pressure measurement is influenced by corneal thickness, among other factors. Eyes with thin corneas tend to have pressures that are under-estimated by tonometry, while eyes with thick corneas tend to have pressures that are over-estimated.
While IOP measurements are important, you must consider whether it’s necessary in the balance of causing more corneal insult, delaying healing or increasing a patient’s chances of corneal infection. A pachymetry test is a simple, quick, painless test to measure the thickness of your cornea. With this measurement, your doctor can better understand your IOP reading, and .In the U.S., the range of typical central cornea thickness (CCT) values is between 540 and 550 micrometers (or microns). However, these figures are estimates. Your provider will consider .
Background and objective Due in part to its effect on intraocular pressure (IOP) measurements, the assessment of central corneal thickness (CCT) is recognized as an essential part of the .Goldmann IOP tends to generate low readings despite very thick corneas. Researchers are studying new parameters that can affect the accuracy of IOP measurements such as corneal .Corneal thickness is particularly important as it affects the measurement of IOP, with thin corneas resulting in underestimated IOP readings, and thick corneas with overestimates. Corneal thickness is also an independent risk . The Message. "It's clear to me that more than any other finding by recent clinical trial, clinicians have embraced and adopted the procedure of measuring central corneal thickness," states Robert D. Fechtner, MD, of the .
IOP measurements obtained with this tonometer have also shown to be influenced by central corneal thickness, with higher IOP readings with thicker corneas. [9] [10] This tonometer has been shown to be affected by other biomechanical properties of the cornea, including corneal hysteresis and corneal resistance factor.The judgment of the influence of corneal thickness by Park et al 1 may have been different if they would have included the results of Kohlhaas et al 4 obtained in 125 eyes and if the influence of age would have been taken in account as well as the influence of the 3 central corneal thickness values >640 μm in Figure 6 of the Kohlhaas et al 4 paper. Park et al lump together .Effects of corneal thickness, corneal curvature, and intraocular pressure level on Goldmann applanation tonometry and dynamic contour tonometry. Ophthalmology. 2007 Jan;114(1):20-6. doi: 10.1016/j.ophtha.2006.06.047.
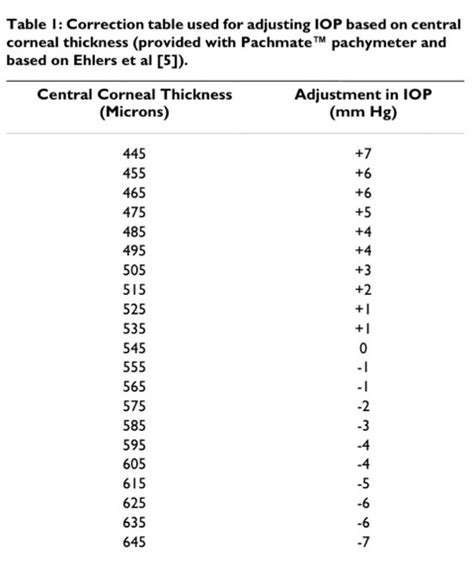
INTRODUCTION. Elevation of intraocular pressure (IOP) is no longer considered a key element in the definition and diagnosis of open-angle glaucoma 1 (OAG), yet it remains the only treatable risk factor and is known to be associated with presence and progression of the disease. 2-5 Although IOP can be misleading on an individual case basis, large population-based surveys . Scattergram of central corneal thickness (CCT) versus intraocular pressure (IOP) of children aged 7 to 18years (r = 0.44, n = 982). The collection between different CCT and IOP, CIOP values According to Doyle's [9] criteria, CCT values were stratified into three groups: thin cornea group (CCT<520 µm), normal thickness cornea group (CCT = 520 .Corneal thickness is particularly important as it affects the measurement of IOP, with thin corneas resulting in underestimated IOP readings, and thick corneas with overestimates. Corneal thickness is also an independent risk factor for the development of glaucoma.In our paper simultaneous IOP measurement by applanation and intracameral tonometry was performed. Assuming a normal CCT of 520 μm, an IOP correction for every 10 μm change in corneal thickness is recommended. But in the Ehlers paper, there are some confusing arguments. Ehlers et al 2 describe a very good correlation between direct and .
Pearson correlation: r=0.16, p=0.049. USP: ultrasound pachymetry. Discussion. Due to its effect on IOP measurements, it is of paramount importance to obtain CCT readings as part of a glaucoma assessment [].Although USP is the most widely utilized CCT measuring method, it is not without its disadvantages [15,18].As a contact procedure, USP carries the risk of infection .
3. Ehlers N, Hansen FK. Central corneal thickness in low-tension glaucoma. Acta Ophthalmol (Copenh). 1974;52:740-6. 4. Von Bahr G. Measurements of the thickness of the cornea. Acta Ophthalmol. 1948;26:247-266. 5. Von Bahr G. Corneal thickness; its measurement and changes. Am J Ophthalmol. 1956;42:251-266. 6. Brubaker R F. Tonometry . When taking an intraocular pressure measurement, the thickness of the cornea will also be measured. Then, the doctor will adjust the pressure measurement accordingly. . Corneal thickness measurements are crucial to prepare for any type of surgery that modifies the cornea. This includes refractive surgery and corneal transplantation.Many clinicians do believe that the effect is due to corneal thickness affecting IOP measurements. People with thinner corneas have real IOP higher than the measured IOP, and it is this difference in measured versus actual IOP that contributes to the increased glaucoma risk. There is also the possibility that thinner corneas indicate a thinner .
pachymetry corneal thickness ranges chart
Measuring intraocular pressure (IOP) is well established, with the Goldmann Applanantion Tonometer (GAT) being the most widely used device. The influence of corneal thickness on IOP by conventional tonometers was acknowledged by Goldmann [] and clarified later by other investigators [2–6].It has been recommended by many that GAT readings should . This method allows the measurement of IOP without deforming the cornea; therefore, its readings are independent of corneal thickness, unlike other methods. [47] [18] [83] Studies have shown DCT to have good precision, reproducibility, and correlatability compared to GAT and other tonometers.
had Tono-Pen IOP measurements. Central Corneal Thickness and Intraocular Pressure Among normal controls, there was a relationship between CCT and IOP (linear regression analysis, P 0.0153; Fig 2). In this model, the IOP increases 2.4 mmHg for every 100- m increase in CCT. Additional analysis of the relationship between IOP and
A healthcare provider uses a pachymetry test to measure the thickness of your cornea. Thickness matters for glaucoma and refractive errors. . which measures intraocular pressure (IOP). Test Details . The equipment generally takes a series of measurements and provides the average as your result. Optical pachymetry. Your provider may use . Intraocular pressure (IOP) or eye pressure is the fluid pressure of the eye. . in which the reduced mean corneal thickness can give rise to an underestimation of IOP measurements taken with GAT. For this reason, the measurement of central corneal thickness is critical for accurately measuring IOP. Normal IOP. Corneal thickness measurement in the management of primary open-angle glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology. 2007; 114:1779-1787. . Comparison of intraocular pressure measurements: Goldmann applanation tonometry, noncontact tonometry, Tono-Pen tonometry and dynamic contour tonometry. Eye (Lond) .
The measurement of intraocular pressure (IOP) is an essential examination in daily ophthalmic procedures, also is a fundamental tool in the management and follow-up of glaucoma patients [].Many factors, such as central corneal thickness (CCT), corneal astigmatism and biomechanical properties of the cornea can affect the accuracy of IOP . The thickness of the cornea is important because it affects the accuracy of intraocular pressure measurements, the success of refractive surgeries, and the diagnosis and management of corneal diseases. . Corneal thickness correction is a procedure that adjusts the intraocular pressure readings to account for the thickness of the cornea, which .INTRAOCULAR PRESSURE (IOP) is an important parameter in the diagnosis and follow-up of glaucoma. While Goldmann applanation tonometry is the preferred method of measurement of IOP, several factors, including corneal thickness, may influence its accuracy. 1 A positive linear correlation between central corneal thickness (CCT) and IOP has been reported by Kruse .
Glaucoma is a disease in which eye pressure (intraocular pressure) can be elevated. Elevated eye pressure can cause nerve fiber loss in the retina which may result in blindness or decreased vision. . Comparison of Central Corneal Thickness Measurements Using Optical and Ultrasound Pachymetry in Glaucoma Patients and Elderly and Young . Background: To assess the impact of knowing central corneal thickness (CCT) on glaucoma management in a United Kingdom district general hospital. Methods: A masked observational non-interventional study included 304 eyes of 152 consecutive glaucoma cases attending general clinic. CCT was measured using a hand-held pachymeter. IOP, as . Accurate measurement of corneal thickness is a prerequisite for providing a precisely corrected IOP. Therefore, it would be important to investigate the reliability of CCT measurements in the TP. Our results showed that TP measurements did not differ significantly from USP measurements: the average difference was 1.22 μm. “OHTS reignited interest in the issue of corneal thickness and IOP measurement,” Dr. Stamper said. (Additionally, it has been recognized that the effects of LASIK surgery render accurate IOP measurement by standard applanation tonometry difficult or impossible.) Since OHTS, doctors are advised to measure corneal thickness along with IOP.
However, corneal hysteresis values can be produced by various combinations of corneal thickness, rigidity, intraocular pressure, and hydration. Corneal resistance factor (CRF) is another measurement provided by ORA and is derived using the .
iop correction for central cornea thickness
vervangen vd vochtmeter in de wasdroger
GAT and ORA (IOPg) readings showed a positive correlation with central corneal thickness (P<0.005). . Schneider E, Grehn F . Intraocular pressure measurement-comparison of dynamic contour .
Corneal pachymetry is the measurement of corneal thickness, done through a simple, quick, painless test to assit in better understanding ophthalmic issues. . Glaucoma is a progressive optic neuropathy that can lead to blindness and one of its primary risk factors is high intraocular pressure (IOP). There are numerous studies that show a link .
vi d6 vochtmeter
iop correction factor chart
webLVDT linear position sensors are readily available that can measure movements as small as a few millionths of an inch up to several inches, but are also capable of measuring positions up to ±30 inches (±0.762 meter). Figure 1 shows the components of a typical LVDT. The transformer's internal structure consists of a primary winding centered .
iop corneal thickness measurements|iop correction factor chart